
Chronic pain is a pathological condition that may prevent people from being able to live full, active, productive lives. It can make even simple tasks difficult, like participating in physical activity, eating properly, working, or enjoying life. Austin Neurosurgeons offers several treatments for this debilitating condition. One of the most effective, long-term treatments for chronic pain syndrome involves the use of a Spinal Cord Stimulation (SCS).
What is Spinal Cord Stimulation (SCS)
Spinal Cord Stimulation (SCS) is a proven, drug-free pain management therapy used by hundreds of thousands of people worldwide. It’s designed to interrupt your body’s own “pain signals” for long-term and often dramatic chronic pain relief.
Neurological Conditions Treated by SCS
Chronic Pain can take many forms and is usually placed in two major categories of its own: chronic pain with an identifiable cause and chronic pain with no identifiable cause. Chronic pain with no identifiable cause is generally used to describe pain that last more that three to six months and is pain that continues even after tissue has fully healed. Pain can establish a pathway in the nervous system in some cases, becoming the problem in and of itself. In other words, the nervous system may be sending a pain signal even though there is no ongoing tissue damage. The nervous system misfires and creates the pain. In such cases, the pain is the disease rather than a symptom of an injury.
Complex regional pain syndrome (CRPS) is an uncommon nerve disorder that causes intense burning pain, usually in the arms, hands, legs or feet. It can occur after an injury, either to a nerve or to tissue in the affected area. Along with pain, the patient may experience extreme skin sensitivity and changes in the color, temperature or moistness of the skin.
Arachnoiditis is a painful condition caused by the inflammation of the arachnoid, one of three linings that surround and protect the brain and spinal cord. The arachnoid can become inflamed due to a variety of reasons including prior surgery, epidural injections, myelograms, and any trauma to the dura. When arachnoiditis begins to impact the nerves, it can cause a number of symptoms, including numbness, tingling and a distinctive stinging and burning pain in the lower back or legs. Other symptoms may include muscle cramps, twitches, spasms and bladder/bowel/sexual dysfunction. There is no cure for this condition, so the goal of treatment is to control pain and symptoms.
Failed back syndrome (FBSS) or post-laminectomy syndrome (lumbar or cervical) is persistent or recurrent pain, mainly involving the lower back and/or legs usually in the distribution of the sciatic nerve. This can sometimes be present even after prior anatomically successful spinal surgery. FBSS is considered a diagnosis of exclusion, so CT scans or MRIs must demonstrate that there are no surgically correctable lesions present. Patients with FBSS often have epidural/ intraneural/perineural fibrosis or scar tissue, which generally will not respond to surgery but may respond to SCS.
Peipheral Neuropathy, Nerve damage, Neuropathy or Neuritis normally occurs when the outer sheathing or the myelin (protective covering) of nerve cells degenerate. There are many conditions and diseases that cause nerve damage. More than 100 types of peripheral neuropathy pain have been identified, each with its own characteristic symptoms. These symptoms depend on the type of nerves involved. Some people may experience temporary numbness, tingling and pricking sensations, sensitivity to touch, or muscle weakness. Others may experience more extreme symptoms, such as burning pain (especially at night), muscle wasting, paralysis or organ or gland dysfunction.
Spinal Cord Stimulator Trials
If you are a suitable candidate for SCS, often the first step is to implant a small trial device temporarily. A thin lead or leads are implanted and are connected to a trial spinal cord stimulator for about one week. The trial stimulator is programmed with stimulation programs customized to the specific areas of the patient’s pain. The trial period is helpful to both the patient and physician for several reasons, including:
- Determines whether SCS effectively relieves pain
- Provides an assessment period to determine which type of SCS technology works best
- Allows for the evaluation of different stimulation settings and programs
SCS Implantation
If the SCS trial provides adequate pain relief, then a permanent system may be implanted. SCS is a reversible therapy, so even though it is called permanent, treatment can be discontinued at any time and the implanted parts turned off and/or removed.
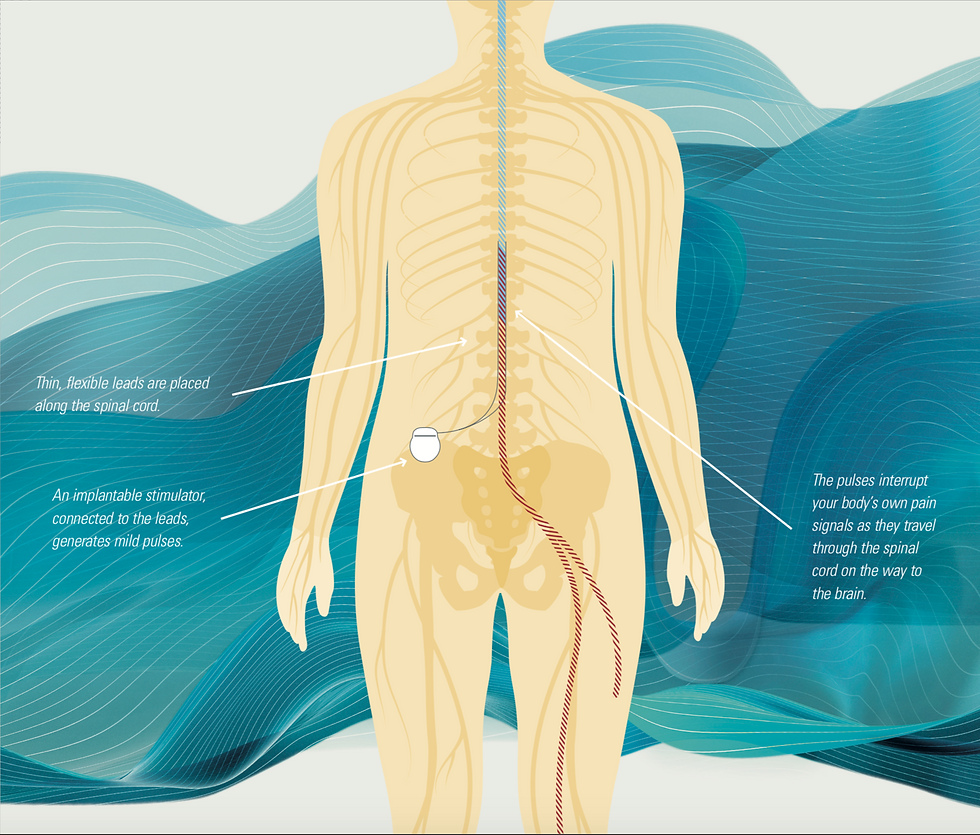
The procedure itself only lasts about 30 min and requires only two small incisions. We prefer our patients be sedated for the procedure to ensure their comfort. A 1 inch incision is made along the spine depending on the area being treated. A second 2 inch incision is made near the buttock to place the battery. The leads are placed in the epidural space above the spinal cord and attached to the battery. Once the leads and battery are in place, tested, and confirmed with imaging, the incisions are closed, local anesthetic injected, and a dressing is applied. Most patients will go home the same day and taught how to program/regulate their device.
Lifting, bending, twisting, and stretching is restricted for two weeks after surgery. But the patient may walk and lightly exercise during that time. The incision takes a few weeks to heal so soaking the incision in bathtubs, pools, hot tubs, lakes, etc is discouraged during that time. The patient may shower but will need to pat dry the area immediately afterward.
Results and Outcomes
Most patients of Austin Neurosurgeons with Dr. Daniel Peterson report significant pain reduction and relief post operatively. Dr. Daniel Peterson, with Austin Neurosurgeons, is one of the leading SCS implantation experts in this growing field. He has also performed more of these procedures than any other Neurosurgeon in the Central Texas region. Contact Austin Neurosurgeons today if you are ready to experience significant improvement in your pain and overall health and wellness.

Comentarios